App Improves Medication Side Effects Monitoring
- January 3, 2022
- William Payne
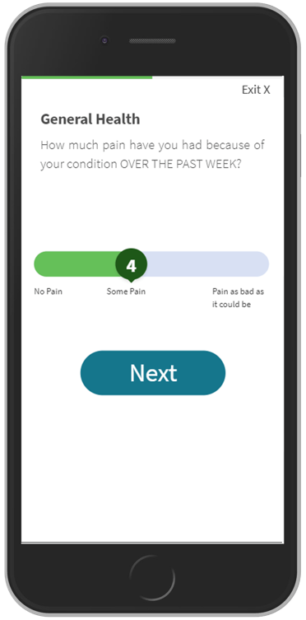
US non-profit CreakyJoints, an advocacy group for arthritis sufferers, has published a peer-review of the use of its ArthritisPower mobile app to capture side-effects of powerful rheumatic disease medications, and the potential of the mobile app to enable doctors to develop improved strategies for patient monitoring.
In the trial, researchers focused on the application of the rheumatic disease medication methotrexate (MTX), specifically for short-term symptoms that are temporally related to dose administration.
Researchers found that nearly two-thirds of rheumatoid arthritis (RA) and psoriatic arthritis (PsA) patients experience methotrexate side effects (including fatigue and nausea) and that for many, the experience of such symptoms is much more intense in the 1-2 days after each weekly dose is taken. The study compared patients’ symptoms measured in the 1-2 days after taking MTX to their symptoms measured several days later.
According to CreakyJoints, the study demonstrates the value of a smartphone-based strategy for remote therapeutic monitoring and that the use of digital technology to assess medication-related symptoms is both feasible and acceptable to patients.
The study, “Patient-Reported Nausea and Fatigue Related to Methotrexate: A Prospective, Self-Controlled Study in the ArthritisPower Registry,” was published in Rheumatology and Therapy (28 Nov. 2021).
Previous studies have confirmed that the Patient Reported Outcomes Measurement Information System (PROMIS) developed by the National Institutes of Health reliably captures important patient experiences across physical, mental, and social health domains. Dozens of PROMIS measures are available in the CreakyJoints’ ArthritisPower Research Registry, which researchers in this study used to collect information about patients’ experience with MTX therapy, a commonly prescribed medication for RA, PsA, and other forms of autoimmune arthritis. MTX has a reasonable effectiveness and safety profile that has been well documented in prior studies but is known to induce unwanted symptoms among some patients who take it.
“In this study, we used a self-controlled case series study design using electronic patient-reported outcome measures (e-PROMs) to generate real-world evidence regarding patients’ experiences and treatment side effects. We found that the majority of current MTX users report side effects, such as fatigue and nausea, with mean changes in these symptoms measured shortly after each weekly dose that exceeds a minimally important difference (MID),” said W. Benjamin Nowell, PhD, Director, Patient-Centered Research, CreakyJoints and principal investigator of ArthritisPower. “While these results may not be particularly surprising and serve to reinforce findings from prior research, it’s noteworthy that we were able to measure the change in symptoms that fluctuate appreciably over the week in relation to the timing of MTX use. While patient-provider interactions occurring during traditional office visits can assess a medication’s effectiveness to improve disease activity over weeks and months, they may miss the mark to capture patients’ real-life experience of taking medications that may involve untoward side effects that vary greatly according to when the treatment is taken. If side effects are perceived by the patient as unmanageable, then patients will forego taking the medication, increasing their risk for disease worsening or complications.”
In the Rheumatology and Therapy study, 85 current MTX users contributed regular e-PROM data within-week of dose administration related to nausea or fatigue, which allowed for correlation of side effect onset and severity with the timing of weekly administration. Among participants, 39.8 percent were on a biologic DMARD and 59.3 percent were on a non-biologic DMARD only. Of the participants reporting MTX-associated nausea at baseline, 41 percent (16/39) experienced worsened nausea using a MID of 3 units. Of the participants reporting MTX-associated fatigue at baseline, 41 percent (21/51) experienced worsened fatigue using an MID of 3 units. Using an alternative cutoff for MID of 5 units, the corresponding proportions were 31 percent (12/39) for nausea and 39 percent (20/51) for fatigue. Net, about one-third of patients in this sample experienced meaningful worsening of nausea or fatigue in the day following their weekly MTX dose, with a magnitude of change exceeding the MID.
“By stratifying the results according to self-reported symptoms measured before assessment began, we were able to quantify the severity of important symptoms that are bothersome to a large minority of patients. These important observations would have been obscured if only reported at a group level. This study’s findings also offer evidence for the convergent validity of the specific PROMIS instruments used in this study, which have not been previously evaluated in RA patients,” said Dr. Jeff Curtis, MD, MS, MPH, Marguerite Jones Harbert – Gene V. Ball Endowed Professor of Medicine in Rheumatology and Immunology at the University of Alabama at Birmingham and co-principal investigator of the ArthritisPower registry.
Dr. Curtis continued, “The magnitude and frequency of temporally related MTX-associated side effects in rheumatoid arthritis patients has been difficult to quantify in the past because traditional assessments are collected in office. This study demonstrates that patients are open to tracking their treatment experience and associated symptoms, remotely, using a smartphone app, thereby providing researchers with new insights regarding the scope of important side effects that may impact adherence. More patients and providers are becoming comfortable with virtual telehealth appointments and remote patient and remote therapeutic monitoring. It’s increasingly apparent that being able to capture PRO data digitally will be essential to understanding the individual patients’ experience of living with arthritis and its management.”
In this study, participants were recruited from within the ArthritisPower Patient-Powered Research Network Registry. To be eligible for the study, ArthritisPower participants need to be residents of the United States aged 19 and older (or aged 21 if from Puerto Rico), with a self-reported physician diagnosis of RA or PsA. After completing a prescreening questionnaire to determine further eligibility, patients currently taking oral MTX were invited to participate in the longitudinal study, which required at least 1 dose taken in the prior month and use of MTX for less than 10 years. In the absence of data indicating a tolerance threshold for duration of MTX therapy, the 10-year limit was chosen to strike a balance between possible adjustment to MTX tolerance over time and enabling adequate participation in the survey. MTX use was permitted either alone (i.e., monotherapy) or in combination with other DMARDs.